Report information
- Author: Hans Jakob
- When : 5 Juli 2021
- About : Extreme tumors of the skin and burn contractures in Congo
Extreme tumors of the skin and burn contractures in Congo
Summary
The specialty of plastic surgery makes surgical interventions in developing countries particularly effective because it does not require extensive diagnostics. Marking, excision, defect coverage with flaps or free grafts; the follow-up care is done by local doctors. Thus, in 2 weeks, 100 to 200 patients can be operated on who otherwise would not have the chance. Some extreme but typical cases of skin tumors are demonstrated.
Introduction
Congo is an absolutely neglected country from a medical point of view, six times larger than Germany, but with a similar 80 million inhabitants still on the same level as Europe 150 years ago. Corruption and 60 years of civil war have prevented any development and especially investment from outside. There are only a few doctors (1:10,000) and, above all, hardly any surgeons, since postgraduate assistants at most African universities have to pay high fees to be allowed to assist. It is therefore not surprising that in sub-Saharan Africa benign and malignant tumors often grow out of control and ultimately kill their carriers.
With an Interplast team, we have been to Goma, a city of 2 million on the border with Rwanda, six times in recent years. Since we were not allowed to operate in any of the 5 local hospitals, we found a blood bank with a poorly furnished operating room with no running water and frequent power outages. Every morning up to 200 patients with their relatives stood in front of the entrance, of whom we were able to relieve 120 to 200 of their external suffering in the 10 days depending on the severity. Committed colleagues assist us in Goma and three of them receive further training as surgeons through the B-Braun Foundation.
The majority of patients had large tumors (facial bony tumors, neck lymphomas, strumen, large keloids) burn contractures, and terminal conditions of tropical infections. Infants with congenital malformations usually do not make it in life. Thus, our urgent tasks included the removal of monstrous facial tumors with subsequent reconstruction, and the resolution of extreme burn contractures. Despite near-perfect follow-up by local colleagues, we often lack late op results, as many patients return to their bushes immediately after surgery.
Education and prevention could sometimes prevent burn scars that disfigure for a lifetime. These contractures occur after third-degree burns, when young children fall into wood fires or are pushed into them by the animals that are often present; however, second-degree scalds more commonly become infected when young children pull themselves up by a kettle of boiling water. Unfortunately, instant cold water therapy is largely unknown worldwide, because any water below 37 degrees takes the burn heat of over 70 degrees out of the skin just as quickly! Wherever children play, there should be a bucket of water next to every fireplace.
Here are some glaring cases demonstrated from Congo, which require a lot of intuition, flexibility and improvisation under the poor diagnostic and operative circumstances there. But that is what makes these interplast missions so interesting and instructive.

Fig. 1a

Fig. 1b
Figs. 1a+b. Infant with congenital giant nevus scheduled for surgery in April 2020. We purchased 3 skin expanders that we will use on our next visit to Goma and instruct the parents in filling. Three to six months later, or when perforation is imminent, the stretched skin is pulled over the excision defect. Free split skin or full thickness skin grafts from the groin unfortunately turn totally black and cause a visual difference.
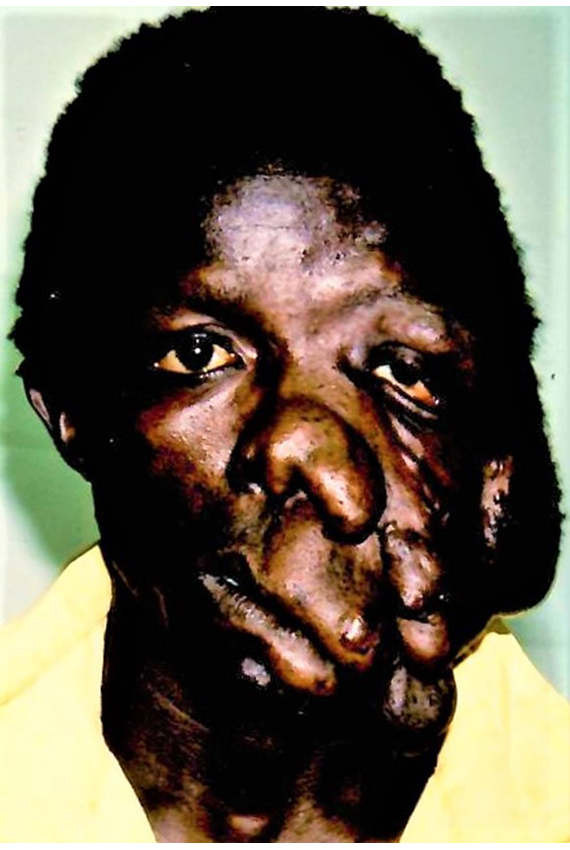
Fig. 2a
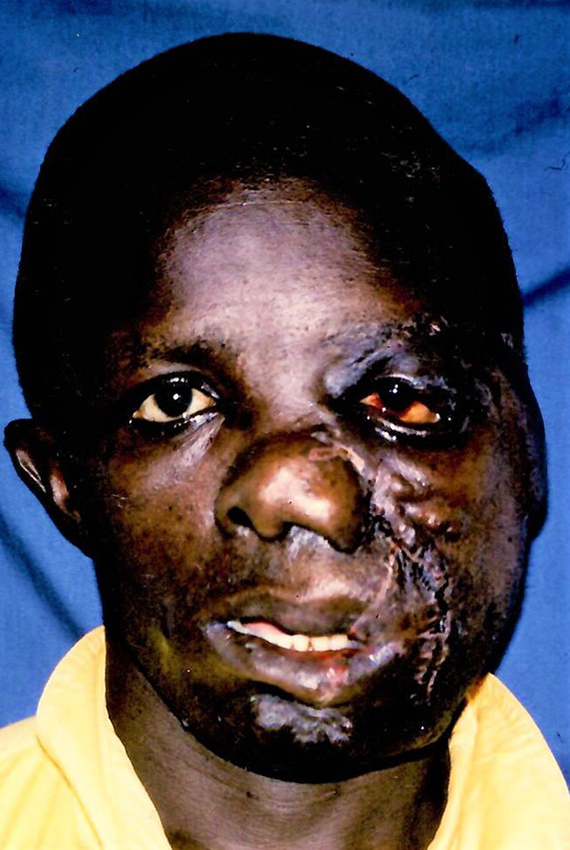
Fig. 2b
Fig. 2a+b. Neurofibromas of the face are among the most difficult plastic surgeries because they are traversed by a network of heavily bleeding arteries and therefore require bold and rapid surgery. Unfortunately, the remaining skin is equally inelastic, so that the initially satisfactory result forces another operation after a few years.

Fig. 3
Fig. 3. No one likes to operate on cavernous hemangiomas, but leaves them to the plastic surgeon. This patient was on the schedule in Goma in April 2020: we want to clamp all protruding caverns individually or together, resect them, and apply waterproof suture rows under the clamps. The thinner the skin, the more inconspicuous the scarring. Growing cavernous hemangiomas in infants and children are best repressed with propranolol and prednisolone.

Fig. 4
Fig. 4. Probable malignant tumor growing for 5 years, which had not broken through the mucosa, so that the large excision defect could be completely covered with the advanced neck skin. Postoperative facial nerve paresis recovered presumably with largely preserved parotid gland.

Fig. 5a

Fig. 5b
Fig. 5a+b. In children, such contracted hands can be stretched without any problems, since no bony stiffening has occurred yet and, surprisingly, the extensor tendons are not burned along with them. In developing countries, these are often primarily second-degree scalds that only become infected in the following weeks, converting to third-degree defects.

Fig. 6a

Fig. 6b
Fig. 6a+b. Congenital varicosis with arteriovenous fistulas that became more pronounced and painful over the years. In two times of bloodlessness (less than 1.5 hours), most of the previously indicated convolutes could be extracted. However, recurrences are to be expected.
According to a presentation at the 7th online scar symposium of the company Juzo (compression stockings) on 24.10.2020 in Berlin.
Katja Kassem-Trautmann, Plastic Surgery Zug, Switzerland
